Osteoporosis
Causes, Symptoms, and Treatment
Updated on: June 2023
Weak, easily broken bones are an epidemic in the United States. They’re often tied to osteoporosis, a disease that causes bones to degenerate over time. This makes them less flexible, more brittle, and easier to break.
According to the International Osteoporosis Foundation, more than 44 million Americans aged 50 and older either have or face the threat of developing osteoporosis due to low bone density levels. Projections put this number at more than 60 million by 2020. Across the world, a fracture due to osteoporosis happens about once every three seconds, causing nearly 9 million fractures—just from stress being put on weak bones.
Osteoporosis is treatable, reversible, and can be prevented for longer periods of time with the knowledge of what it is and how to attack it. So let’s dig into osteoporosis to find out what it is, how to notice it, its causes, and what to do once you or a loved one have it.
Find What You Need
What is Osteoporosis?
Osteoporosis is a degenerative bone disease that causes the loss of bone mass and bone tissue. Over the course of your life, old bone is removed from your body through a process called resorption, and new bone replaces it through formation, according to the National Resource Center for Osteoporosis and Other Bone Diseases.
However, there comes a time when your body can no longer keep up with the amount of bone you are losing. Most humans reach their “peak bone mass” in their early 20s, and then your body slowly (very slowly) starts lose more bone than it creates. This process takes a long time, though, especially when it comes to impacting the strength of your bones. The resource center also says that the process of resorption usually starts to outpace the process of formation by the time you hit 30, whether you’re a man or a woman. In most cases, men develop more bone over the course of their lives than women do, which leaves women more susceptible to suffering from osteoporosis.
Osteoporosis has onset once your bones get to a point where they are brittle, weaker, and easily broken. There are little to no symptoms of the disease, so easily breaking a bone may be the first sign that you have osteoporosis.
Osteoporosis is a large reason why seniors falling is such a big deal. If bones become easier to break, they also become a lot harder to heal, because not as much bone is being created to heal the fracture. The longer bones take to heal—especially hips and legs—the longer the elderly have to stay in the hospital. Longer hospital stays have been proven to show increased rates of mortality. They are related to increased complications while you’re in the hospital, because you’re more likely to develop more issues the longer you stay. You can even reach a point where your bones are no longer able to completely heal themselves, which causes issues with normal daily routines for the rest of your life.
How Does Osteoporosis Develop?
Osteoporosis can develop from a wide range of reasons, some of them medical (like autoimmune diseases, cancer and mental illness), and some of them from medications you take that can have bone loss as a side effect. This is why more than 10 million people have been officially diagnosed with osteoporosis. Let’s take a look at what exactly causes it to develop.
Medical Causes
The main cause of osteoporosis is other medical conditions, which either hinder the body from creating bone at a necessary rate or contribute to the speed at which bone deteriorates. The types of medical conditions that foster the development of osteoporosis are vast, covering various cancers, autoimmune diseases, and more. Let’s take a look at some of these issues.
Menopause
One demographic most at risk for developing osteoporosis is postmenopausal women. During the menopause process, women experience a dramatic decrease in hormones being produced by their bodies, and this can result in bone loss.
While researchers aren’t completely sure why menopause is directly related lower bone density, the connection is there, especially in the first couple years following the ceasing of periods. Some women lose nearly half their bone density in the decade following menopause. Treatment for bone loss needs to be taken seriously and efficiently during the menopausal process, because women already have smaller bones.
Cancer
The effect cancer has on the skeletal system is two-sided: the cancer itself affects the deterioration of your bones, and many treatments for cancer (chemotherapy, steroids, etc.) can also inhibit bone loss. Also, a 2013 study points out that “the skeleton is also the most common site of metastatic disease,” which is the most advanced type of cancer. This is due to osteoblasts and osteoclasts—the two main parts of the bone that focus on formation and resorption, respectively—inhibiting the rapid advancement of cancer cells, the study says.
Some of the main cancers that reap osteoporosis as a main side effect include breast and prostate cancers. Premenopausal women who receive chemotherapy for breast cancer have been shown to start the menopausal process almost a decade earlier than the average (early 50s), according to the aforementioned study. Both the menopause process—as we just discussed—and the treatment for menopause and breast cancer can all contribute to the proliferation of osteoporosis. Similarly, men who develop prostate cancer have similar issues with a hormone imbalance, which affects bone growth and development.
Low Calcium Levels
Calcium is the most important mineral in our body when it comes to bone strength. Calcium is constantly replaced in your bones to help keep them flexible and sturdy, so low calcium levels can result in weaker and brittle bones. Low calcium levels can stem from a variety of reasons, including:
- Poor diet, especially as a child. The stronger and bigger your bones become in your youth (with the help of calcium), the more bone you have to potentially lose as you age.
- Gastrointestinal surgery, which can impact how your body can absorb necessary nutrients like calcium, according to the Mayo Clinic.
- Hypocalcemia, a calcium deficiency disease that can come about from aforementioned reasons like dieting or medications, or from genetic reasons.
Autoimmune Diseases
There are certain autoimmune diseases that, if present, can increase the risk of osteoporosis, both because of their direct effects on the body and the medications used for treatment. These autoimmune diseases include:
Rheumatoid Arthritis:
Aside from the medication used for rheumatoid arthritis—a disease that affects the joints all around your body—increasing your chances for osteoporosis, the inactivity caused by the condition can contribute to bone loss. The less certain parts of the skeletal system are used, like your wrists and hips for lifting weights and exercising, the more likely you are to lose bone density in those areas.
Lupus:
Similar to rheumatoid arthritis, lupus—an autoimmune disease where the body attacks, inflames, and damages certain organs like your skin, joints, and tissues—can be a risk factor to osteoporosis through inactivity. The less you use these parts of your body, which can be in great pain due to the disease, the less chance your bones have to remain strong and healthy.
Celiac disease:
This disease makes the body reject gluten, a protein largely found in wheat and rye products. If left untreated, the disease can affect your stomach and intestines’ ability to function and absorb the nutrients it needs, like calcium, which can then affect how strong and dense your bones are.
Medications
In addition to the medical reasons for why osteoporosis develops, there are also a slew of medicines you may be taking that aid in its development. Some are used to help combat the very diseases that are causing bone loss, like cancer. It’s a vicious cycle, but it’s also important to know what kinds of medicine have bone loss as a side effect. Let’s take a look at some of the medications that contribute to osteoporosis, courtesy of a 2014 study:
Steroids:
Known in the medical world as glucocorticoids, these are used to treat conditions like lupus, allergies, rashes, autoimmune diseases, and plenty more. The aforementioned study notes that 30 to 50 percent of those who use these medications develop fractures, and that steroids can cause a range of bone density-decreasing habits like accelerating bone resorption and supporting fractures before bone density levels have even decreased to osteoporosis levels. Medication that helps prevent osteoporosis works well to combat osteoporosis-via-steroids.
Proton pump inhibitors:
PPIs, which are used to help fight acid reflux, have shown to increase the risk of fractures, though it’s not clear why. The correlation is there, though, and in 2010, the FDA made PPIs come with a warning of an increased risk of fractures in certain areas of the body.
Type 2 diabetes medication:
The study pointed out that certain medications used to treat type 2 diabetes—specifically, certain thiazolidinediones—have features that prevent the body from recognizing when it needs to create new bone, which can then lead to osteoporosis.
Epilepsy medication:
Medicine used to help combat epilepsy—a disease that provokes random seizures—has shown to contribute to the reduction of bone density in people of all ages, but it largely affects postmenopausal women and those over the age 65. Studies in animals have shown antiepilepsy medication inhibits certain receptors that contribute to the proliferation of bone growth.
MPA (birth control/hormonal control):
This specific medication is most commonly used for birth control and hormone replacement therapy for menopausal women, but it also contributes to the rapid loss of bone mass within a couple years of using it. The study pointed out, though, that bone loss suffered from MPA is reversible.
Aromatase inhibitors:
These are used for hormone therapy is perimenopausal and postmenopausal women and “promote accelerated bone loss” due to the loss in estrogen, according to the study.
The Hormone Health Network notes that other medications used to treat medical issues can also contribute to the development of osteoporosis, and these include medications used to treat:
- Various Cancers
- Heart Burn
- Heart failure
- Blood-clot Prevention
- The Prevention of Organ transplant rejection
Given the wide range of medications that have osteoporosis as a side effect, it’s important you keep your dosage under control. Take the least amount of medicine you have to for the least amount of time possible. Don’t take the medications that cause osteoporosis unless your doctor prescribes them for a lengthy period of time. If you do need these medications for a long time, consult your doctor about how you can combat unhealthy side effects like osteoporosis.
Lifestyle Causes
How active you are and the kinds of food and drink you consume play into how likely you are of developing osteoporosis. Whether they can be explained by researchers or not, some of the following lifestyle habits have been proven to contribute to increased levels of bone loss:
- Excessive alcohol consumption
- Tobacco use
- Inactive lifestyle (not regularly exercising)
- Diet lacking in vitamin C and vitamin D
Osteoporosis can stem from many facets of life. Whether it’s a medical reason or medication you’re using to combat those medical issues or just a plain old lifestyle, how do you know if you’re suffering from the condition?
Symptoms of Osteoporosis
One major issue with osteoporosis is that its symptoms and effects don’t show up until it has progressed to the point where it’s a hindrance. “People don’t take it seriously because it’s a silent disease,” said Dr. Clarita S. Ketels, an internal medicine doctor at Watson Clinic in Lakeland, Fla. “You don’t feel the bone loss.”
This is why it’s important to take preventative steps and be in constant contact with your doctor if you fit the description of someone who is particularly at a higher risk of developing the disease (white postmenopausal women, people of Asian ancestry, etc.). Some warning signs that you may have osteoporosis include:
- Poor and slouchy posture
- Brittle bones (bones that break easy or from minimal force)
- Loss in height, either from the loss in bone or slouched posture
- Back pain caused from easily fractured vertebrates and the curving and weakening of the spine
When you suffer a slight fracture or a break, it’s called a stress fracture, which are very tiny cracks in bones that can occur when the bones are weaker and suffer from slight traumas like falling down or bumping into hard surfaces. These symptoms will creep up on you, so it’s important you take easily fractured bones and a change in posture and height seriously.
Who is at a Greater Risk of Developing Osteoporosis?
The older you get, the more likely you are to develop osteoporosis. This is simply due to the longevity of life paired with how long the degradation of bone in the body outpaces the formation of bone. Around 30, bone stops being produced at a higher rate than it is being resorbed, so the longer you live, the less bone you are likely to have. One study found that 70 percent of fractures are sustained by seniors, those 65 and older.
But this doesn’t mean that all older people will develop osteoporosis—some are far more likely than others due to characteristics like race, gender, ethnicity, and family history. Some factors that play into the likelihood of developing osteoporosis include:
Gender:
Women are far more likely to develop osteoporosis than men, primarily because men develop more bone over their lives, thus they have more bone to lose. Women—especially shorter and smaller women—have less bone to lose, so bone density levels typically drop below normal more quickly than men. Women also have other medical conditions, like menopause and certain cancers, that contribute to the development of osteoporosis.
Race:
Caucasian people and people of Asian descent are more likely to develop osteoporosis than other races
Smokers and drinkers: People who smoke tobacco and drink in excess have been shown to have a greater risk of developing osteoporosis. Smoking can cause an endless list of cancer, which directly causes osteoporosis, and alcohol prevents the body from absorbing calcium, which can help build stronger bones.
Family history:
If your immediate family members have suffered from osteoporosis, you are more likely to develop the condition than someone who hasn’t had family members suffer from it. You may have a similar, thinner body frame as your mom, which can be passed down. There are other issues related to osteoporosis (certain diseases, menopausal symptoms) that you can inherit, which then increase your chance of developing the condition.
The most important step in understanding how to handle osteoporosis is getting ahead of the disease with prevention and treatment, but how do you know if you’re even in danger?
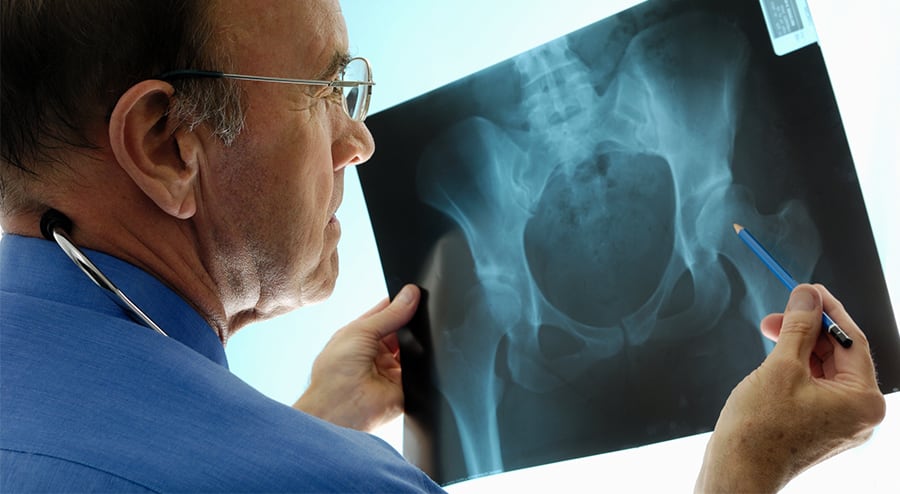
Testing for Osteoporosis
Large medical and osteoporosis associations around the United States agree that the best way to test for osteoporosis is a dual-energy X-ray absorptiometry scan, known as a DXA. This test finds levels of bone density in various parts of your body, like your arms and hips. It then reveals a certain number, which is compared to other bone density levels of people your age, race, and body size. If your levels are more than 2.5 standard deviations (also known as a T-score) below the average, then you are classified as having osteoporosis.
The DXA test gives very accurate readings, and is more accurate than a standard X-ray, which can muddle results and show that bones are slightly bigger than they actually are. It also emits far less radiation than a standard X-ray and is painless. It takes less than 15 minutes, too, so you can know your results right away and get started on a treatment plan.
What is Osteopenia?
Just because your bone mass is lower than it should be doesn’t mean you have full-blown osteoporosis. There’s a diagnosis that sits between normal bone density and extremely low levels, and that is osteopenia. This means that your T-score levels sit between one and 2.5 standard deviations below the average bone density levels.
The Harvard Medical School says that about half of Americans older than 50 are affected by osteopenia. HMS also stresses that you should still take the necessary steps needed to help combat bone loss, even if your T-score number is higher than what is classified as osteoporosis.
“The label (of which disease you have) matters less than the (T-score) number. These distinctions are to some extent arbitrary lines in the sand,” said Dr. Maureen Connelly, a preventative medicine expert at Harvard. Typically, the treatment and prevention plans for both disease are the same with a focus on trying to fight bone loss and restore bone density levels as close to normal as possible.
Prevention and Treatment of Osteoporosis
While osteoporosis may not be noticeable until bones start breaking, it’s possible to prevent rapid bone loss and help build strong bones. “Changes that occur in the skeleton, if they are at a troublesome level, can be dramatically improved upon by aggressively managing the condition,” said Dr. Ethel Siris, a member of the National Osteoporosis Foundation (NOF).
There are treatments available for osteoporosis and the one you choose depends on what is causing the loss of bone. Also, doctors will typically prescribe a medication that will stop bone from deteriorating so quickly while also activating bone growth. These medicines can include:
- Fosamax
- Actonel
- Evista
- Boneva
- Forteo
You may also receive supplements to help combat the medical issue that may be causing the bone loss, such as calcium deficiency, a vitamin D deficiency, or menopause (the loss of hormones). In these cases, doctors will tailor your prescription to the severity of mineral or hormone deficiency.
In addition to treatment of bone density levels, there are some proactive steps you can take before levels get too low—or if they’ve reached the point where you need treatment. Here are some lifestyle steps you can take in order to fight bone loss:
- Reduce alcohol consumption
- Introduce more protein to your diet, whether it be through supplements or healthier food
- Lose weight to help put less stress on your bones
- Exercise through cardiovascular activities and lifting weights. Both of these help maintain healthy and strong bones
The NOF also notes that treatment and prevention plans vary based on age and gender, not just on how severe bone density levels are. These plans are flexible, just like healthy bones.